- Details
- Description
-
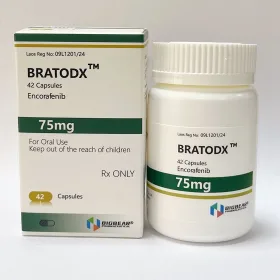
Packaging Size50Capsule
-
Strength150mg
-
CompositonCeritinib
-
TreatmentALK positive metastatic NSCLC
-
FormCapsule
-
BrandCerini
-
Quantity Unit150mg*50C
-
ManufacturerTongmeng (Lao) Pharmaceutical & Food Co., Ltd.(TLPH)
Ceritinib is a prescription-only drug used for the treatment of non-small cell lung cancer (NSCLC).
Non-Small Cell Lung Cancer
Indicated for the treatment of patients with metastatic non-small cell lung cancer (NSCLC) whose tumors are anaplastic lymphoma kinase (ALK)-positive as detected by an FDA-approved test
450 mg PO qDay with food
Continue until disease progression or unacceptable toxicity
Also see administration
Dosage Modifications
Dose reduction increments
- Starting dose: 450 mg qDay
- First dose reduction: 300 mg qDay
- Second dose reduction: 150 mg qDay
- Unable to tolerate 150 mg/day: Discontinue