- Details
- Description
-
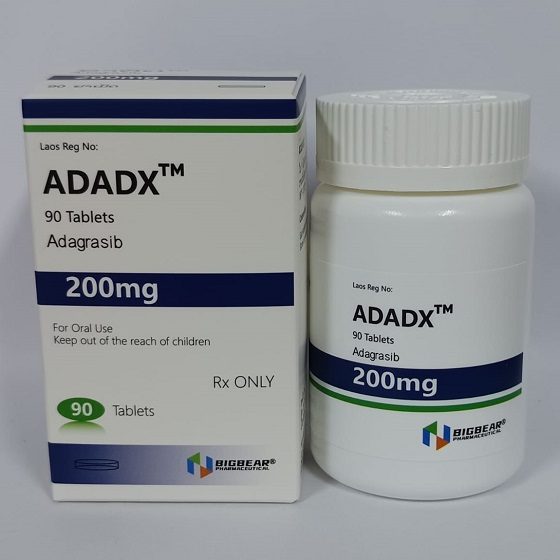
Packaging Size90T/bottle
-
Strength200mg
-
CompositonAdagrasib
-
TreatmentKRAS G12C–mutated ocally advanced or metastatic non–small cell lung cancer (NSCLC) or metastatic colorectal cancer (CRC)
-
FormTablets
-
BrandADADX
-
Quantity Unit200mg*90T/box
-
ManufacturerBIGBEAR Pharma,Laos PDR
About Adagrasib
Adagrasib is a prescription medicine used in adults:
alone to treat non-small cell lung cancer (NSCLC)
- that has spread to other parts of the body or cannot be removed by surgery, and
- whose tumor has an abnormal KRAS G12C gene, and
- who have received at least one prior treatment.
in combination with a medicine called cetuximab to treat colon or rectal cancer (CRC)
- that has spread to other parts of the body or cannot be removed by surgery, and
- whose tumor has an abnormal KRAS G12C gene, and
- who have previously received certain chemotherapy medicines.
Your healthcare provider will perform a test to make sure that Adagrasib is right for you.
It is not known if Adagrasib is safe and effective in children.
Non–Small Cell Lung Cancer
Indicated for KRAS G12C–mutated locally advanced or metastatic non–small cell lung cancer (NSCLC) in adults who have received ≥1 systemic treatment
600 mg PO BID until disease progression or unacceptable toxicity
Colorectal Cancer
Indicated in combination with cetuximab for KRAS G12C–mutated locally advanced or metastatic colorectal cancer (CRC) in adults who have received prior treatment with fluoropyrimidine-, oxaliplatin-, and irinotecan-based chemotherapy
600 mg PO BID until disease progression or unacceptable toxicity
In a clinical trial, adagrasib was given with cetuximab
- 500 mg/m2 IV q2wks, or
- 400 mg/m2 IV once followed by 250 mg/m2 IV once weekly
Dosage Modifications
Dosage reductions for adverse reactions
- First dose reduction: 400 mg PO BID
- Second dose reduction: 600 mg PO qDay
- Unable to tolerate 600 mg qDay: Permanently discontinue
Nausea or vomiting
- Grade 3 or 4 despite providing supportive care (eg, antiemetic therapy)
- Withhold until recovery to Grade ≤1 or return to baseline
- Resume at next lower dose level
Diarrhea
- Grade 3 or 4 despite providing supportive care (eg, antidiarrheal therapy)
- Withhold until recovery to Grade ≤1 or return to baseline
- Resume at next lower dose level
QT interval prolongation
-
Corrected QT (QTc) absolute value >500 msec OR an increase >60 msec from baseline
- Withhold until QTc <481 msec or return to baseline
- Resume at next lower dose level
-
Permanently discontinue
- Torsade de pointes
- Polymorphic ventricular tachycardia
- Signs or symptoms of serious or life-threatening arrhythmia
Hepatotoxicity
- Grade 2 AST/ALT: Decrease to next lower dose level
-
Grade 3 or 4 AST/ALT
- Withhold until recovery to Grade ≤1 or return to baseline
- Resume at next lower dose level
-
Permanently discontinue
- AST/ALT >3x ULN with total bilirubin >2x ULN in the absence of alternative causes
Interstitial lung disease (ILD) or pneumonitis (any grade)
- Suspected ILD/pneumonitis: Withhold therapy
- Confirmed ILD/pneumonitis: Permanently discontinue
Other adverse reactions
-
Grade 3 or 4
- Withhold therapy until Grade ≤1 or return to baseline
- Resume therapy at next lower dose level
Renal impairment
- Mild to severe (CrCl 15 to <90 mL/min): No dosage adjustment necessary
Hepatic impairment
- Mild to severe (Child-Pugh A to C): No dosage adjustment necessary
Dosing Considerations
Monitoring Parameters
- Monitor ECGs and electrolytes before initiating, during treatment, and as clinically indicated in patients with congestive heart failure, bradyarrhythmias, electrolyte abnormalities, and in patients who are unable to avoid drugs known to prolong the QT interval
- Monitor AST, ALT, alkaline phosphatase, and total bilirubin before initiating and monthly for 3 months or as clinically indicated; perform more frequent testing in patients who develop transaminase elevations
- Monitor for new or worsening respiratory symptoms (eg, dyspnea, cough, fever) during treatment