- Details
- Description
-
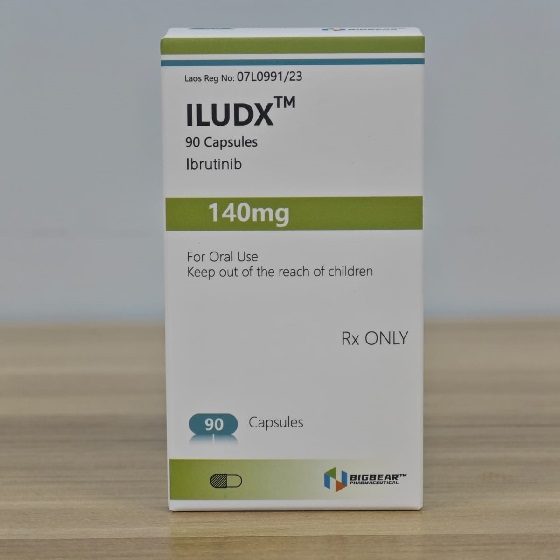
Packaging Size90C/bottle
-
Strength140mg
-
CompositonIbrutinib
-
TreatmentChronic Lymphocytic Leukemia(CLL),Small Lymphocytic Lymphoma(SLL),Mantle Cell Lymphoma(MCL),Waldenström Macroglobulinemia(WM),Marginal Zone Lymphoma(MZL),Graft vs Host Disease(cGVHD)
-
FormCapsules
-
BrandILUDX
-
Quantity Unit140mg*90C/Bottle
-
ManufacturerBIGBEAR Pharma,Laos PDR
Ibrutinib is in a class of medications called kinase inhibitors. It works by blocking the action of the abnormal protein that signals cancer cells to multiply. This helps stop the spread of cancer cells.
Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma
Also indicated for CLL/SLL in patients with 17p deletion
Monotherapy or in combination with rituximab or obinutuzumab, or with bendamustine and rituximab (BR) combination: 420 mg PO qDay
Continue until unacceptable toxicity or disease progression
Mantle Cell Lymphoma
Indication was voluntary withdrawn in the U.S. by manufacturer on April 10, 2023
The decision was made to remove the indication after overall survival (OS) was similar when comparing ibrutinib or placebo in combination with bendamustine and rituximab for mantle cell lymphoma in the phase 3 SHINE trial
Failure to meet this requirement led to the decision to remove the indication after consulting the FDA
Waldenström Macroglobulinemia
Indicated as monotherapy or in combination with rituximab
420 mg PO qDay
Continue until disease progression or unacceptable toxicity
Marginal Zone Lymphoma
Indication was voluntary withdrawn in the U.S. by manufacturer on April 10, 2023
The decision was made to remove the indication after the phase 3 SELENE trial failed to reach its primary endpoint of progression free survival (PFS) when comparing ibrutinib to placebo in combination with bendamustine and rituximab or rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone in patients with previously untreated MZL
Failure to meet this requirement led to the decision to remove the indication after consulting the FDA
Chronic Graft vs Host Disease
Indicated for chronic graft versus host disease (cGVHD) in adults who failed >1 lines of systemic therapy
420 mg PO qDay
Continue until cGVHD progression, recurrence of an underlying malignancy, or unacceptable toxicity
If therapy is no longer required, consider discontinuing therapy based on medical assessment of individual patient
Dosage Modifications
Grade 2 cardiac failure
- Evaluate benefit-risk before resuming treatment
-
MCL and MZL
- First occurrence: Restart at 420 mg qDay
- Second occurrence: Restart at 280 mg qDay
- Third occurrence: Discontinue therapy
-
CLL/SLL, WM, and cGVHD
- First occurrence: Restart at 280 mg qDay
- Second occurrence: Restart at 140 mg qDay
- Third occurrence: Discontinue therapy
Grade 3 cardiac arrhythmias
-
MCL and MZL
- First occurrence: Restart at 420 mg qDay
- Second occurrence: Discontinue therapy
-
CLL/SLL, WM, and cGVHD
- First occurrence: Restart at 280 mg qDay
- Second occurrence: Discontinue therapy
Grade ≥3 cardiac failure or Grade 4 cardiac arrhythmias
- First occurrence: Discontinue therapy
Nonhematological and hematologic toxicities
- Other Grade 3 or 4 nonhematological toxicities
- Grade 3 or 4 neutropenia with infection or fever
- Grade 4 hematological toxicities
-
MCL and MZL
- First occurrence: Restart at 420 mg qDay
- Second occurrence: Restart at 280 mg qDay
- Third occurrence: Discontinue therapy
-
CLL/SLL, WM, and cGVHD
- First occurrence: Restart at 280 mg qDay
- Second occurrence: Restart at 140 mg qDay
- Third occurrence: Discontinue therapy
Coadministration with CYP3A inhibitors
- Moderate CYP3A4 inhibitor: Reduce ibrutinib to 420 mg qDay; modify dose as recommended
-
Reduce ibrutinib dose to 280 mg qDay when coadministered with the following
- Voriconazole 200 mg BID
- Posaconazole suspension 100 mg qDay, 100 mg BID, or 200 mg BID
- Modify dose as recommended
-
Reduce ibrutinib dose to 140 mg qDay when coadministered with the following
- Posaconazole suspension 200 mg TID or 400 mg BID
- Posaconazole IV injection 300 mg qDay
- Posaconazole delayed-release tablets 300 mg qDay
-
Avoid coadministration
- Other strong CYP3A inhibitors (boceprevir, clarithromycin, cobicistat conivaptan, danoprevir and ritonavir, diltiazem, elvitegravir and ritonavir, idelalisib, indinavir and ritonavir, itraconazole, ketoconazole, lopinavir and ritonavir, nefazodone, nelfinavir, paritaprevir and ritonavir and [ombitasvir and/or dasabuvir], ritonavir, saquinavir and ritonavir, tipranavir and ritonavir, and troleandomycin)
- If these inhibitors will be used short term (eg, anti-infectives for <7 days), interrupt ibrutinib
- After discontinuation of a CYP3A inhibitor, resume previous dose of ibrutinib
Hepatic impairment
- Modify dose based on following ULN unless of non-hepatic origin or due to Gilbert’s syndrome
-
Total bilirubin (TB) level >1.5 to 3x ULN
- ≥1 to <12 years: Reduce to 80 mg/m2 PO qDay
- ≥12 years: Reduce to 140 mg PO qDay
- TB >3x ULN: Avoid use
Renal impairment
Mild-to-moderate (eCrCl ≥25 mL/min): No dosage adjustment necessary
Severe (eCrCl <25 mL/min) or patients on dialysis: Not studied